One of the most significant challenges we are facing in Endodontics is treating cases with resorption.
There are different types of resorption, and they each require distinct approaches for successful management. The case I treated below was a case with an internal resorptive defect.
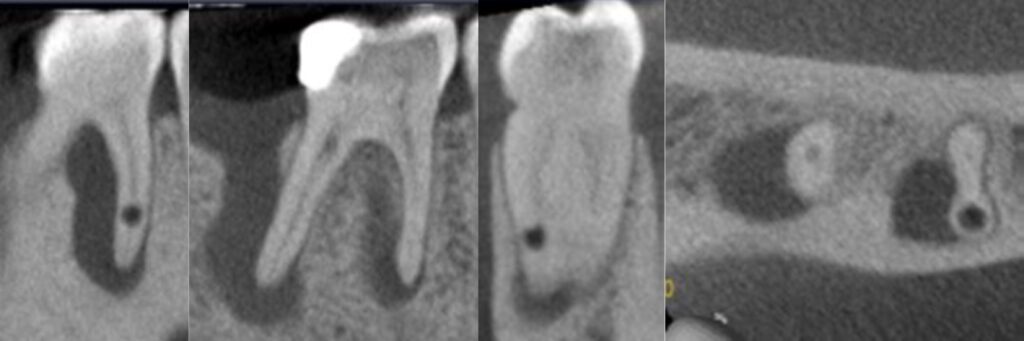
This occurs when the pulp tissue starts resorbing the dentin from the inside out. It can be diagnosed through radiographs, taken with different angulation, showing a well-defined radiolucent area within the tooth. However, the most accurate way to assess whether the resorption is internal or external is by taking a CBCT scan.
Although most of the times it is much easier to treat an internal resorptive defect when compared to an external one, the challenge lies in the management of the infection and maintaining the integrity of the tooth. Early detection is critical to prevent further damage of the tooth.
Endodontic treatment of LR6 – internal resorption
Referral details
The GDP referred the patient for endodontic treatment of his LR6 as a resorptive defect was radiographically detected.
Patient complaint
The patient reported that over the last 5 years he has been experiencing episodes of swelling in his gums with no associated pain.
Clinical Examination
On clinical examination the LR6 was restored with a DO composite.
The tooth was not tender to percussion. Palpation of the adjacent buccal mucosa elicited normal responses. The LR6 gave negative response to cold testing with Endo Ice and delayed positive response to the electric pulp tester. The latter could be a false positive response. Soft tissue examination revealed the presence of a small swelling and a patent suppurating sinus in the soft tissues buccal to the LR6. Periodontal examination revealed no probing defects around the LR6.

Radiographic Examination
Scan analysis showed that the LR6 has two roots with three canals. There was a small circular internal resorptive defect at mid-apical level of the MB canal. The scan showed presence of a large periradicular radiolucency at the mesial root apex, which extended up to the furcation. There was also a large sized radiolucency at the distal root apex which extended coronally and through the LR7 socket that had recently been extracted.
Diagnosis
Chronic periapical periodontitis with suppuration was made for the LR6 due to pulp necrosis and canal contamination with also presence of internal resoprtion.
Treatment options and plan
The following treatment options were discussed with the patient for the LR6:
- Monitor;
- Extraction with or without prosthetic replacement;
- Root canal treatment, subject to restorability assessment.
Root Canal retreatment plan
First appointment
– Consent form for RCT LR6 obtained.
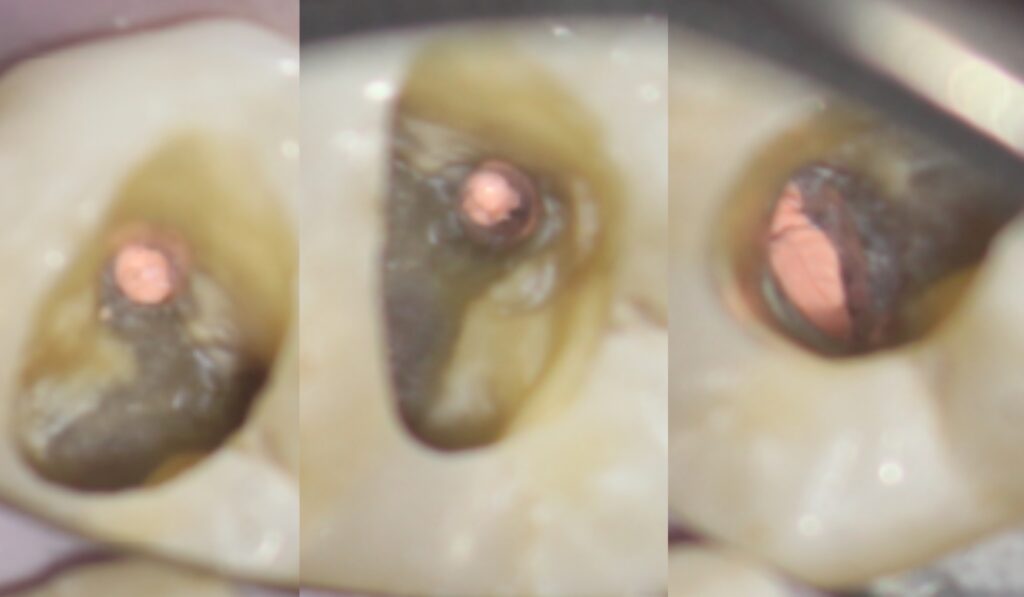
– The tooth was accessed under rubber dam isolated and the access cavity was assessed with the aid of the microscope; no crack was detected.
– Three canals were located and patency was achieved.
– The canals were cleaned, disinfected and prepared for filling. The disinfection was enhanced with the usage of an XP Endo Finisher file especially in the MB canal in order to clean out the internal resorptive defect.
-Calcium hydroxide was used as an interappointment medicament.
Second appointment
– The patient reported that his tooth remained asymptomatic and clinically the swelling and sinus had healed.
– Obturation was carried out using a warm vertical compaction technique.
– The canals’ orifices were sealed with GIC plugs and the access was filled with composite.

Pre and Post Op X-Rays

Pre Op Sinus and Pulp Stones
Post Op Images
Seven-month review
– The patient happily reported that the tooth remained asymptomatic since treatment was completed and the sinus had not reappeared.
– The tooth was not tender to percussion. Palpation of the adjacent buccal mucosa elicited normal responses.
– Radiographic examination showed complete resolution of the radiolucency around the mesial root apex with just remaining widening of the PDL space and a decrease in the size of the radiolucency around the distal root apex, indicating that healing is progressing well.
– Treatment was considered to be successful for the LR6 with incomplete healing.
Post Op X-Ray

Review X-Ray
Personal Reflection
The tooth was a strategic molar given the loss of the LR7 due to fracture 10 years ago. The filling had some depth and could have caused the pulpal issue, but given the history, the presence of an internal crown fracture was also suspected. Analysis of the scan though showed no evidence that this could have propagated down into the root system with the crestal circumferential PDL spaces intact.
The positive EPT reading suggested that there could still be some vital tissue present which could be fuelling the internal resorption, although the readings could be false positives. Early intervention was certainly recommended in this case to avoid further tooth tissue loss and complications of the resorption perforating the mesial or distal root walls.
The patient accepted the recommendations and as he wished to save his tooth, he wanted to proceed with the treatment. Further clinical examination showed no evidence of a fracture and therefore we carried on with the endodontic treatment.
Regarding the management of the internal resorptive defect, I used the XP Endo Finisher in this case, in order to increase the efficacy of the irrigants and deliver them to this inaccessible with files area. Warm vertical compaction technique was also necessary to ensure the internal resorptive defect can be sealed three-dimensionally.
With the aims of the treatment achieved I would expect further apical healing.
